Abstract
Background: Peripheral T-cell lymphomas (PTCL) are a heterogeneous group of hematologic malignancies associated with poor outcomes. Identification of novel prognostic biomarkers might improve current risk stratification. Herein, we aim to evaluate the prognostic value of the neutrophil-to-lymphocyte ratio (NLR), red blood distribution width (RDW-CV), and serum albumin in PTCL and propose a novel risk stratification model.
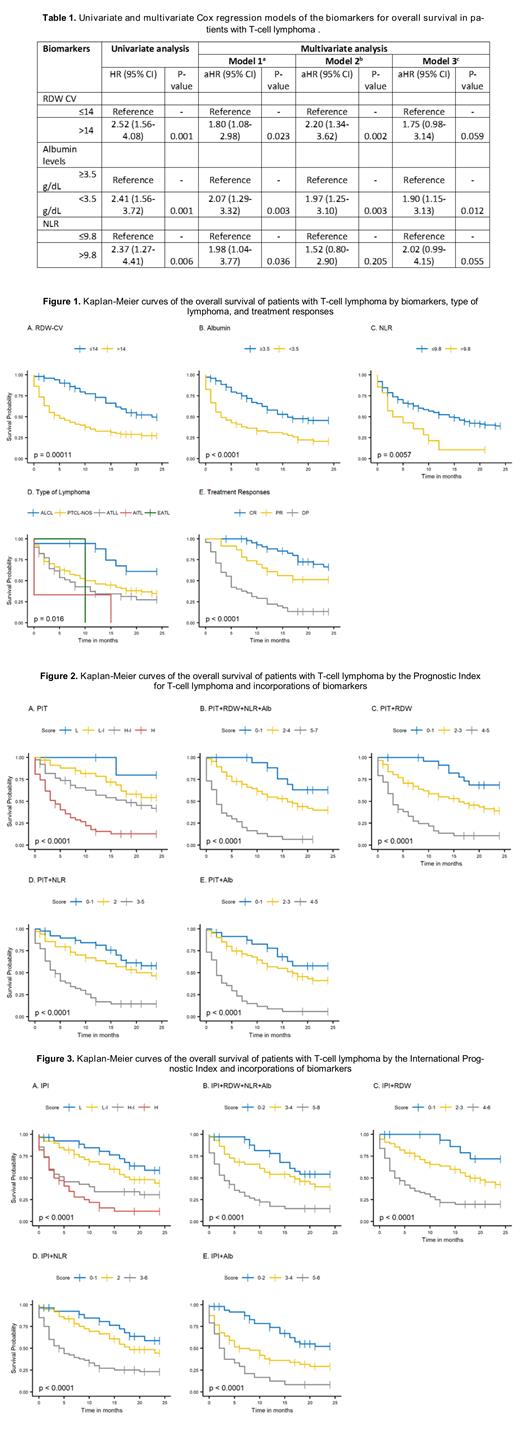
Methods: We performed a cohort study by retrospectively reviewing the medical records of patients with pathologically confirmed PTCL between March 2010 and March 2019. Cutoffs for RDW-CV (≤14 versus >14), serum albumin levels (≥3.5 versus <3.5 gr/dL), and NLR (≤9.8 versus >9.8) were determined by ROC analysis. The IPI and PIT scores were used for risk stratification. We used the Kaplan-Meier method to estimate overall survival (OS) probabilities and the log-rank test to compute their statistical difference. Univariate and multivariate Cox regression analyses were used to estimate hazard ratios (HRs) with a 95% confidence interval (CI). The C-index was used to determine the discriminatory power for each model. Outcomes with a p-value <0.05 were considered statistically significant.
Results: A total of 143 patients were identified. The median age at diagnosis was 62 years old (range 16-93) with a male predominance (62.2%). PTCL, not otherwise specified was the most common subtype (54.7%), followed by adult T-cell leukemia/lymphoma (30.4%), and anaplastic large cell lymphoma (12.2%). We identified a worse 2-year OS for patients with RDW-CV >14 (27% vs. 51%, p<0.0001), serum albumin <3.5 gr/dL (20% vs. 47%, p=0.004), and NLR >9.8 (11% vs. 40%, p<0.0001) (Table 1 and Figure 1). The multivariate analysis showed that only albumin level <3.5 gr/dL (HR: 1.9, 95% CI: 1.15-3.13, p=0.012) was independently associated with poor survival. The PIT score was a better predictor for OS than the IPI score (C-index: 0.705 versus 0.682) (Figure 2A and 3A). The addition of RDW-CV, serum albumin levels, and NLR to the IPI score improved the OS prediction (C-index: 0.692) compared to the IPI score alone (C-index: 0.682). The addition of the above biomarkers to the PIT score slightly improved the OS prediction than the PIT score alone (C-index: 0.706 versus 0.705, respectively) (Figure 2B-E and 3B-E).
Conclusion: In this large cohort of PTCL patients, serum albumin <3.5 gr/dL was an independent negative prognostic biomarker for survival. Furthermore, the addition of this biomarker, RDW, and NLR improved the predictive value of the IPI score and to some extent that of the PIT score. The PIT score had a better stratification power than the IPI score. We are currently validating our findings in a prospective cohort of PTCL patients and to improve clinical decision-making in those deemed to have high-risk disease.
Castillo: Abbvie: Consultancy, Research Funding; BeiGene: Consultancy, Research Funding; Pharmacyclics: Consultancy, Research Funding; Janssen: Consultancy; Roche: Consultancy; TG Therapeutics: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal